230x Filetype XLS File size 2.58 MB Source: ahca.myflorida.com
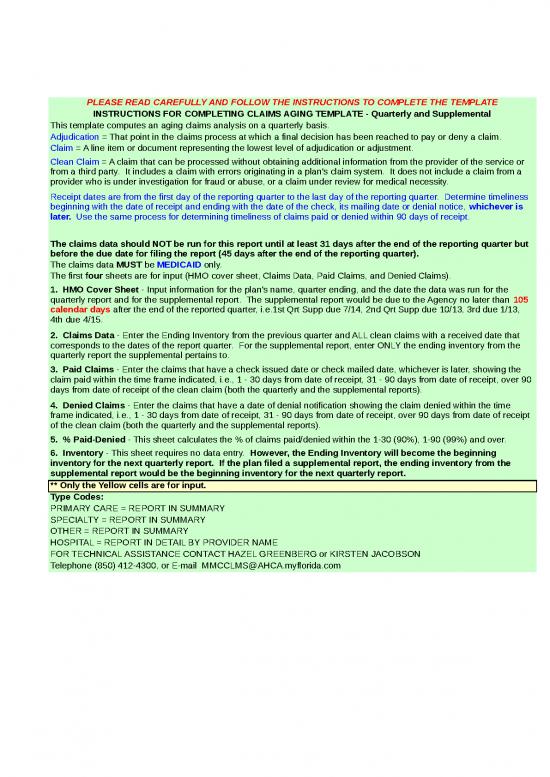
PLEASE READ CAREFULLY AND FOLLOW THE INSTRUCTIONS TO COMPLETE THE TEMPLATE
INSTRUCTIONS FOR COMPLETING CLAIMS AGING TEMPLATE - Quarterly and Supplemental
This template computes an aging claims analysis on a quarterly basis.
Adjudication = That point in the claims process at which a final decision has been reached to pay or deny a claim.
Claim = A line item or document representing the lowest level of adjudication or adjustment.
Clean Claim = A claim that can be processed without obtaining additional information from the provider of the service or
from a third party. It includes a claim with errors originating in a plan's claim system. It does not include a claim from a
provider who is under investigation for fraud or abuse, or a claim under review for medical necessity.
Receipt dates are from the first day of the reporting quarter to the last day of the reporting quarter. Determine timeliness
beginning with the date of receipt and ending with the date of the check, its mailing date or denial notice, whichever is
later. Use the same process for determining timeliness of claims paid or denied within 90 days of receipt.
The claims data should NOT be run for this report until at least 31 days after the end of the reporting quarter but
before the due date for filing the report (45 days after the end of the reporting quarter).
The claims data MUST be MEDICAID only.
The first four sheets are for input (HMO cover sheet, Claims Data, Paid Claims, and Denied Claims).
1. HMO Cover Sheet - Input information for the plan's name, quarter ending, and the date the data was run for the
quarterly report and for the supplemental report. The supplemental report would be due to the Agency no later than 105
calendar days after the end of the reported quarter, i.e.1st Qrt Supp due 7/14, 2nd Qrt Supp due 10/13, 3rd due 1/13,
4th due 4/15.
2. Claims Data - Enter the Ending Inventory from the previous quarter and ALL clean claims with a received date that
corresponds to the dates of the report quarter. For the supplemental report, enter ONLY the ending inventory from the
quarterly report the supplemental pertains to.
3. Paid Claims - Enter the claims that have a check issued date or check mailed date, whichever is later, showing the
claim paid within the time frame indicated, i.e., 1 - 30 days from date of receipt, 31 - 90 days from date of receipt, over 90
days from date of receipt of the clean claim (both the quarterly and the supplemental reports).
4. Denied Claims - Enter the claims that have a date of denial notification showing the claim denied within the time
frame indicated, i.e., 1 - 30 days from date of receipt, 31 - 90 days from date of receipt, over 90 days from date of receipt
of the clean claim (both the quarterly and the supplemental reports).
5. % Paid-Denied - This sheet calculates the % of claims paid/denied within the 1-30 (90%), 1-90 (99%) and over.
6. Inventory - This sheet requires no data entry. However, the Ending Inventory will become the beginning
inventory for the next quarterly report. If the plan filed a supplemental report, the ending inventory from the
supplemental report would be the beginning inventory for the next quarterly report.
** Only the Yellow cells are for input.
Type Codes:
PRIMARY CARE = REPORT IN SUMMARY
SPECIALTY = REPORT IN SUMMARY
OTHER = REPORT IN SUMMARY
HOSPITAL = REPORT IN DETAIL BY PROVIDER NAME
FOR TECHNICAL ASSISTANCE CONTACT HAZEL GREENBERG or KIRSTEN JACOBSON
Telephone (850) 412-4300, or E-mail MMCCLMS@AHCA.myflorida.com
Plan Name:
Plan 7 Digit Base
Medicaid ID#:
Contact Person:
Telephone:
Fax:
E-Mail:
MEDICAID CLAIMS ANALYSIS
For the quarter ending:
**Quarterly Report Data Run Date:
***Supplemental Report Data Run Date:
**NOTE: Please enter the date the data was run in
order to capture any claims received near the end of the
report quarter and paid/denied within 30 days of the end
of the report quarter. Quarterlies are due 45 days from
the end of reporting quarter, Supplementals are due
105 days from the end of the reporting quarter.
Comments/Notes:
TOTAL CLEAN CLAIMS AGING BY PROVIDER TYPE 7 Digit ID:
Quarter Ending: Supplemental
Quarterly Run Date: Run Date:
Prior Quarter Clean
Ending Claims TOTAL CLEAN
PROVIDER: Inventory Received CLAIMS
PRIMARY CARE 0
SPECIALTY 0
OTHER 0
HOSPITALS:
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
TOTAL CLEAN CLAIMS AGING BY PROVIDER TYPE 7 Digit ID:
Quarter Ending: Supplemental
Quarterly Run Date: Run Date:
Prior Quarter Clean
Ending Claims TOTAL CLEAN
PROVIDER: Inventory Received CLAIMS
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
no reviews yet
Please Login to review.