210x Filetype XLS File size 0.17 MB Source: www.health.ny.gov
Sheet 1: Phase 3 Catch-All
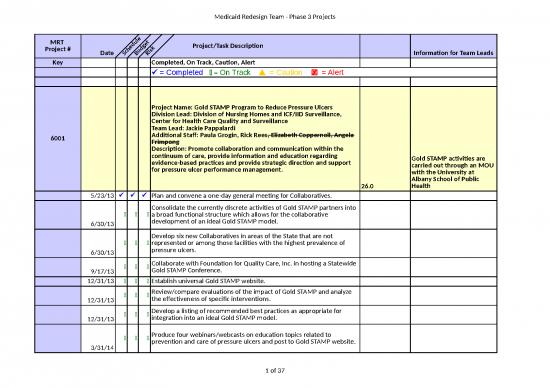
| MRT Project # |
Date | Schedule | Budget | Risk | Project/Task Description | Information for Team Leads | |
| Key | Completed, On Track, Caution, Alert | ||||||
| P = Completed 8 = On Track ▲ = Caution T = Alert | |||||||
| 6001 | Project Name: Gold STAMP Program to Reduce Pressure Ulcers Division Lead: Division of Nursing Homes and ICF/IID Surveillance, Center for Health Care Quality and Surveillance Team Lead: Jackie Pappalardi Additional Staff: Paula Grogin, Rick Rees, Elizabeth Coppernoll, Angela Frimpong Description: Promote collaboration and communication within the continuum of care, provide information and education regarding evidence-based practices and provide strategic direction and support for pressure ulcer performance management. |
26.0 | Gold STAMP activities are carried out through an MOU with the University at Albany School of Public Health | ||||
| 5/23/13 | P | P | P | Plan and convene a one-day general meeting for Collaboratives. | |||
| 6/30/13 | 8 | 8 | 8 | Consolidate the currently discrete activities of Gold STAMP partners into a broad functional structure which allows for the collaborative development of an ideal Gold STAMP model. | |||
| 6/30/13 | 8 | 8 | 8 | Develop six new Collaboratives in areas of the State that are not represented or among those facilities with the highest prevalence of pressure ulcers. | |||
| 9/17/13 | 8 | 8 | 8 | Collaborate with Foundation for Quality Care, Inc. in hosting a Statewide Gold STAMP Conference. | |||
| 12/31/13 | 8 | 8 | 8 | Establish universal Gold STAMP website. | |||
| 12/31/13 | 8 | 8 | 8 | Review/compare evaluations of the impact of Gold STAMP and analyze the effectiveness of specific interventions. | |||
| 12/31/13 | 8 | 8 | 8 | Develop a listing of recommended best practices as appropriate for integration into an ideal Gold STAMP model. | |||
| 3/31/14 | 8 | 8 | 8 | Produce four webinars/webcasts on education topics related to prevention and care of pressure ulcers and post to Gold STAMP website. | |||
| 3/31/14 | 8 | 8 | 8 | Continue to support the six previously established Collaboratives when necessary or requested. | |||
| 3/31/14 | 8 | 8 | 8 | Begin development of a Gold STAMP best practice model. | |||
| 6002 | Project Name: Balancing Incentive Program Division Lead: Mark L. Kissinger Team Lead: Karen M. Ambros Additional Staff: Karen M. Meier, Becky A. Corso, Jennifer C. Alhart Description: Administrative Requirements- Develop Final Work Plan |
||||||
| 5/31/13 | P | P | P | Prepare and send CMS answers to their questions. | |||
| 6/13/13 6/20/13 |
8 | 8 | 8 | Participate in training webinar conducted by TA. | |||
| 7/5/13 | 8 | 8 | 8 | Hire BIP project manager (IPRO). | |||
| 7/31/13 | 8 | 8 | 8 | Prepare first draft of detailed workplan (CMS format). | |||
| 8/8/13 | 8 | 8 | 8 | Revise workplan based on interagency comments. | |||
| 8/21/13 | 8 | 8 | 8 | Submit final draft to Chamber, DOB. | |||
| 8/30/13 | 8 | 8 | 8 | Submit to CMS. | |||
| 6003 | Project Name: Federal Revenue from Additional Emergency Medicaid Claiming and Other Possible Efforts Division Lead: DFRS Team Lead: Phil Mossman Additional Staff: Maria Payne, Woo Hwang, FMG Description: Aliessa population is claimed as FNP except for emergency services. However, none of the emergency services provided to Aliessa inidividuals in a managed care setting are claimed as FP. This project will identify and submit these services to FP. |
||||||
| 3/1/13 | P | P | P | Complete fiscal analysis for calendar years 2011/2012 and begin discussions with CMS | |||
| 6/15/13 | P | P | P | Request formal approval and waiver of two year claim limitation from CMS | |||
| 06/30/13 | P | P | P | Submit claim for federal match for calendar years 2011 and 2012 | |||
| 09/30/13 | 8 | 8 | 8 | Submit claim for federal match for January 1-March 31, 2013 | |||
| 10/01/13 | 8 | 8 | 8 | Establish separate premium groups for Aliessa individuals to be effective April 1, 2013 | |||
| 6004 | Project Name: PCMH Savings Division Lead: DPDM Team Lead: Greg Allen Additional Staff: Description: Eliminate payments for 2008 PCMH recognized Level 2 providers and reduce payments from $6 pmpm to $5 pmpm for 2008 PCMH recognized Level 3 providers. Assumes that some providers will meet 2011 standards to receive incentive payment. |
||||||
| 10/1/13 | 8 | 8 | 8 | Evolution project to edit the eMedNY to implement PCMH changes into the system | |||
| 6005 | Project Name: Increase Efficiency of Transportation Utilization by Transportation Manager Division Lead: Div of Program Development and Management Team Lead: Mark Bertozzi Additional Staff: Tim Perry-Coon, Heidi Seney, Lani Rafferty Description: Achieve savings in transportation management by accelerating migration to livery and public transportation as appropriate. Improve quality and transportation through administrative actions against low performing providers. |
Completed April 2013. | |||||
| 1/30/13 | P | P | P | Develop livery and other lower cost alternatives to transportation with Transportation Managers | |||
| 2/1/13 | P | P | P | Identify initial group of low performing transportation providers | |||
| 2/16/13 | P | P | P | Transportation Manager to hire Utilization Review manager | |||
| 2/20/13 | P | P | P | Provide information on low performing transportation providers to DLA, OHIP Operations and OMIG | |||
| 3/1/13 | P | P | P | Ambulatory assessment of transportation use and needs | |||
| 3/5/13 | P | P | P | Initial meeting with OHIP Operations and OMIG staff to discuss evidence based performance records of selected providers | |||
| 3/22/13 | P | P | P | Reach agreement with OMIG on administrative actions against low performing transportation providers | |||
| 4/1/13 | P | P | P | Take administrative action against low performing transportation providers | |||
| 4/1/13 | P | P | P | Begin implementation of lower cost modes of transport | |||
| 6006 | Project Name: Managed Care Efficiency Adjustment Division Lead: Division of Finance & Rate Setting/Bureau of Managed Care Reimbursement Team Lead: Megan Ryan/Mike Dembrosky Additional Staff: Phil Mossman/Stephanie Fargnoli Description: Generate $50M gross savings ($25M State share) by implementing Plan specific quality rate adjustment in Managed Care premiums |
$25.00 | |||||
| DATA ANALYSIS | |||||||
| 4/19/13 | P | P | P | Complete plan specific & regional analysis on Inpatient metrics (PQIs, PPRs, PPCs) | DQPS | ||
| 8 | 8 | 8 | Aggregate all quality metrics on a plan specific & regional basis | Mercer | |||
| EDUCATION | |||||||
| 4/1/13 | P | P | P | 3M webinar with the Plans on the 3M suite of potentially preventable metrics | 3M/DFRS | ||
| 8 | 8 | 8 | Present ambulatory metrics to the Plans at Monthly Policy and Planning Meeting or a separate webinar | 3M | |||
| 8 | 8 | 8 | Present PPC analysis to the Plans at Monthly Policy and Planning Meeting | DQPS | |||
| 8 | 8 | 8 | Present aggregated plan specific & regional information and discuss approaches to incorporate into the premiums at the Monthly Policy and Planning Meeting or an interim meeting | DFRS | |||
| METHODOLOGY/RATE DEVELOPMENT | |||||||
| 8 | 8 | 8 | Discuss/determine interaction with other quality metrics currently reflected in the premiums | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Discuss/determine whether aggregate or individual metrics will be utilized and how they will be treated in determining Plan's adjustment | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Discuss/determine whether benchmark for adjustment will be Statewide, Regional or a percentage of the same | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Discuss/determine the frequency of future updates and update to the base data | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Discuss/determine whether a performace incentive will be considered in future adjustments | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Discuss/determine how the adjustment will be incorporated into the premium | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Decide how new adjustment will interact with the existing Mercer efficiency adjustment (LANE, PPA) and the impact on the 2% ATB | DOH/Mercer with 3M consultation | |||
| 8 | 8 | 8 | Complete modeling the adjustment by Plan; by region | DFRS | |||
| 8 | 8 | 8 | Provide data to Mercer for consideration in the rate range | DFRS | |||
| 8/9/13 | 8 | 8 | 8 | Mercer to provide rate range information to the Department | Mercer | ||
| 8/28/13 | 8 | 8 | 8 | DOH to complete build up the July Rates with efficiency adjustment | DFRS | ||
| 8/29/13 | 8 | 8 | 8 | Provide rates to DOB and CMS for approval | DFRS | ||
| 8/30/13 | 8 | 8 | 8 | Brief plans on July Rates, which will include the efficiency adjustment | DFRS | ||
| 9/13/13 | 8 | 8 | 8 | Receive DOB and CMS approval | -- | ||
| 9/13/13 | 8 | 8 | 8 | Transmit July Rate package to EmedNY for payment | DFRS | ||
| DEBRIEF/NEXT STEPS | |||||||
| Complete | Pulling data for metrics | ||||||
| Ongoing | Running metrics | ||||||
| Ongoing | collapsing metrics | ||||||
| Ongoing | Update/refine methodology for future adjustment | ||||||
| 6007 | Project Name: Reduce Accounts Receivable Balances Division Lead: John Ulberg/Ann Foster Team Lead: Phyllis Stanton, John Gahan Additional Staff: Adele Compton, Donna Choiniere, Robert Loftus, Tim Casey, Jason Corvino, Terry Provost Description: Implement an aggressive recovery program to reclaim Accounts Receivable liabilities from providers over the next 18 months. |
$50.0 | |||||
| 02/22/13 | P | P | P | Develop a summary document which outlines the specifics of the proposal and circulate to DOB/FMG for review and comment. | |||
| 02/22/13 | P | P | P | Meet with DOB and FMG to assess the feasibility of the proposal. Decide if statute is required or if proposal can be implemented administratively. | |||
| 04/01/13 06/01/13 | P | P | P | Compile a list of current Accounts Receivable balances by provider and the payment option selected by each. | |||
| 04/30/13 06/20/13 | 8 | 8 | 8 | Distribute a letter to notify providers about the change in the State's collection policy and the date by which they will notify DOH which payment option they select. | |||
| 07/31/13 09/30/13 | 8 | 8 | 8 | Finalize all provider collections for Option #1 - paid in full by 9/01/13 (interest waived). | |||
| 03/31/14 | 8 | 8 | 8 | Finalize all provider collections for Option #2 paid in full by 3/01/14 (50% interest waived). | |||
| 03/31/15 | 8 | 8 | 8 | Finalize all provider collections for Option #3. | |||
| 6008 | Project Name: Reduce Accounts Receivable Balances (Part B) Division Lead: John Ulberg/Ann Foster Team Lead: Phyllis Stanton Additional Staff: Kevin Wright, Mark Shutts, Adele Compton, Michelle Levesque Description: Implement a process to collect Accounts Receivable liabilities that currently do not have recoupment procedures in place. |
||||||
| P | P | P | Identify providers with liabilities that currently do not have a recovery structure in place. | ||||
| 08/01/13 | P | P | P | Develop a list of Providers for Grp #1 (Change of Ownership) to determine which liabilities can be transferred to new owner | |||
| 09/01/13 | 8 | 8 | 8 | Work with FMG and Counsel's Office on solutions for recovery methods. | |||
| 11/01/13 | 8 | 8 | 8 | Implement recovery procedures for providers in group #1 (providers still in business, but is billing under a different provider i.d.) | |||
| 12/01/13 | 8 | 8 | 8 | Begin efforts with OMIG and Attorney General's Office to collect liabilities for providers in group #2 (providers no longer in business). Need to determine if liabilites are collectible. | |||
| 3/31/14 | 8 | 8 | 8 | Develop and implement provider-specific recovery plans for group #3 (providers with no recoupment percentage in the system) | |||
| 6009 | Project Name: Accelerate MLTC Enrollment Division Lead: DLTC Team Lead: Mark Kissinger Additional Staff: Margaret Willard Description: Accelerate FFS to MLTC transition |
||||||
| 4/1/13 | P | P | P | Secure approval for the LTHHCP population to move into MLTC in Westchester, Nassau, Suffolk and NYC | |||
| 8 | 8 | 8 | Work with Maximus to evaluate the people who are falling off the path to auto-assignment | ||||
| 4/5/13 | P | P | P | Move private duty nursing population into MLTC | |||
| 5/1/13 8/1/13 | 8 | 8 | 8 | Evaluate enrollment plan to expedite additional counties with capacity | |||
| 5/10/13 7/1/13 | 8 | 8 | 8 | Evaluate remaining personal care population in NYC | |||
| 6010 | Project Name: Develop Initiatives to Integrate and Manage Care for Dual Eligibles (Fully Integrated Duals Advantage - FIDA) Division Lead: DLTC Team Lead: Mark Kissinger, Rebecca Corso Additional Staff: John Ulberg, Ken Evans Description: Develop approaches for serving dual eligibles |
||||||
| 6/6/13 6/26/13 7/24/13 |
8 | 8 | 8 | Resolution of outstanding MOU issues | |||
| 6/15/13 | 8 | 8 | 8 | Develop Base Data - Summarize Historical Data | |||
| 6/30/13 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 6/30/13 | 8 | 8 | 8 | Release of NYS Data Book (Phase 3 - 2011) | |||
| 7/1/13 7/2/13 | 8 | 8 | 8 | Finalize MOU between CMS/NYSDOH | |||
| 7/8/13 | 8 | 8 | 8 | CMS and State release draft Readiness Review tool to plans | |||
| 7/15/13 | 8 | 8 | 8 | Issue desk review letter to begin readiness review process | |||
| 7/15/13 | 8 | 8 | 8 | Develop Base Data - Remove costs for historical HR&R funds embedded in the raw data, adjust for IBNR claims | |||
| 8/1/13 | 8 | 8 | 8 | Plans submit documentation for desk review (Phase 1) | |||
| 8/8/13 | 8 | 8 | 8 | Plans submit documentation for desk review (Phase 2) | |||
| 8/15/13 | 8 | 8 | 8 | Adjust base data for any changes to the populations and or financial impacts that may have taken place from the base period to the rate period | |||
| 9/15/13 | 8 | 8 | 8 | CMS reviews draft desk review deficiencies | |||
| 9/30/13 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 10/1/13 | 8 | 8 | 8 | Present rate development to stakeholders | |||
| 10/1/13 | 8 | 8 | 8 | Letters to plans to correct desk review deficiencies | |||
| 10/15/13 | 8 | 8 | 8 | Plans submit responses to correct desk review deficiencies | |||
| 10/15/13 | 8 | 8 | 8 | Establish a finalized methodology for rate setting | |||
| 10/31/13 | 8 | 8 | 8 | Medicaid rates finalized | |||
| 11/1/13 | 8 | 8 | 8 | Three-way Contracts shared with plans and the State for signature | |||
| 11/7/13 | 8 | 8 | 8 | Site visits (including systems testing) | |||
| 11/15/13 | 8 | 8 | 8 | Pre-enrollment validation (e.g., filling vacant positions, website, phone lines) | |||
| 12/1/13 | 8 | 8 | 8 | State and Plan signed Three-way Contract returned to CMS | |||
| 12/1/13 | 8 | 8 | 8 | Brief FIDA plans on new rates | |||
| 12/31/13 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 1/1/14 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 1/3/14 | 8 | 8 | 8 | Final Readiness Review Determination | |||
| 1/15/14 | 8 | 8 | 8 | Publish PMPM for the Demo | |||
| 1/31/14 | 8 | 8 | 8 | Plans establish connectivity with CMS enrollment, payment systems | |||
| 2/1/14 | 8 | 8 | 8 | Marketing begins to community-based LTSS beneficiaries and plans begin to accept opt-in enrollments (Phase 1) | |||
| 3/31/14 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 4/1/14 | 8 | 8 | 8 | Opt-in enrollment takes effect for community-based LTSS participants (Phase 1) | |||
| 4/1/14 | 8 | 8 | 8 | Adjust the Base data for the SNF population | |||
| 5/1/14 | 8 | 8 | 8 | 60-day beneficiary notices sent for community-based LTSS passive enrollment (Phase 1) | |||
| 6/1/14 | 8 | 8 | 8 | 30-day beneficiary notices sent for community-based LTSS passive enrollment (Phase 1) | |||
| 6/30/14 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 7/1/14 | 8 | 8 | 8 | Passive enrollment takes effect for community-based LTSS participants (Phase 1) | |||
| 7/1/14 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 7/1/14 | 8 | 8 | 8 | Establish and Publish a revised PMPM including SNF Residents | |||
| 8/1/14 | 8 | 8 | 8 | Marketing begins to facility-based LTSS beneficiaries and plans begin to accept opt-in enrollments (Phase 2) | |||
| 9/30/14 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 10/1/14 | 8 | 8 | 8 | Opt-in enrollment takes effect for facility-based LTSS participants (Phase 2) | |||
| 11/1/14 | 8 | 8 | 8 | 60-day beneficiary notices sent for facility-based LTSS passive enrollment (Phase 2) | |||
| 12/1/14 | 8 | 8 | 8 | 30-day beneficiary notices sent for facility-based LTSS passive enrollment (Phase 2) | |||
| 12/31/14 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 1/1/15 | 8 | 8 | 8 | Passive enrollment takes effect for facility-based LTSS participants (Phase 2) | |||
| 1/1/15 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 3/31/15 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 6/30/15 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 7/1/15 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 9/30/15 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 12/31/15 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 1/1/16 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 3/31/16 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 6/30/16 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 7/1/16 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 9/30/16 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 12/31/16 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 1/1/17 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 3/31/17 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 6/30/17 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 7/1/17 | 8 | 8 | 8 | Submit 6-month progress report to CMS | |||
| 9/30/17 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 12/31/17 | 8 | 8 | 8 | Quarterly stakeholder engagement | |||
| 6011 | Project Name: OPWDD Fully Integrated Duals Advantage - FIDA Division Lead: DLTC Team Lead: Mark Kissinger, Rebecca Corso Additional Staff: John Ulberg, Ken Evans Description: Develop approaches for serving dual eligiblesin OPWDD |
||||||
| 10/31/13 | 8 | 8 | 8 | MOU Development | |||
| 3/31/14 | 8 | 8 | 8 | Related activities | |||
| 6012 | Project Name: DSRIP - Public Hospital Transformation Division Lead: Greg Allen/Division of Program Development and Management Team Lead: Lana Earle, Lyn Hohmann Additional Staff: Phil Mossman Description: Development of metrics and framework for the transformation of the public hospitals in NYS to meet unmet needs and align with the healthcare goals of the NYSDOH. Defining metrics and a framework that CMS will approve, allowing NYS to move forward with DSRIP and related projects. |
||||||
| 8/1/2013 | 8 | 8 | 8 | Finalize State Metrics | |||
| 5/29/2013 | ü | ü | ü | Set up meeting with Jacqueline Matson and Liz Villamil to review DSRIP and metrics | |||
| 5/29/2013 | ü | ü | ü | Establish plan for finalizing metric set in alignment with NYS QAAR and other | |||
| 6/12/2013 | ü | ü | ü | Finalize metric set for submission to CMS | |||
| 6/17/2013 | ü | ü | ü | Submit proposed metric set with rationale to CMS | |||
| 7/1/2013 | 8 | 8 | 8 | CMS Review, discussion of proposed metric set | |||
| 7/15/2013 | 8 | 8 | 8 | Revision of metric set done and submitted to CMS | |||
| 8/1/2013 | 8 | 8 | 8 | CMS Review and acceptance of metric set | |||
| 9/1/2013 | 8 | 8 | 8 | Finalize development of public hospital strategies | |||
| 5/29/2013 | ü | ü | ü | Identify key leads in all public hospitals and associations | |||
| 6/5/2013 | ü | ü | ü | Compile most current plans from each public hospital | |||
| 6/12/2013 | ü | ü | ü | Planning meeting with and association leads | |||
| 6/30/2013 | 8 | 8 | 8 | Review and ID weaknesses/strengths/alignment with metrics | |||
| 7/15/2013 | 8 | 8 | 8 | Face to face meeting with key leads of each public to lay out metric set, strategies and anticipated framework for monitoring. | |||
| 8/9/2013 | 8 | 8 | 8 | Follow-up a. HHC, b. Public Hospital, c. SUNY strategy set with weekly calls--alignment of quality/financial aspects | |||
| 8/9/2013 | 8 | 8 | 8 | Public Hospitals submit strategy CMS - ready for final department review | |||
| 8/13/2013 | 8 | 8 | 8 | Final in-house review | |||
| 9/1/2013 | 8 | 8 | 8 | Submit to CMS | |||
| 12/2/2013 | 8 | 8 | 8 | Financial strategy | |||
| 8/1/2013 | 8 | 8 | 8 | Identify funding requests from participating entities and MRT initiatives | |||
| 9/1/2013 | 8 | 8 | 8 | Submission of financial request to CMS | |||
| 12/2/2013 | 8 | 8 | 8 | Work with Council/DLA to develop written agreements with participating entities | |||
| 9/1/2013 | 8 | 8 | 8 | Establish framework for monitoring strategies including reporting and evaluation of metrics | |||
| 6/12/2013 | ü | ü | ü | Identify with OQPS model for reporting and evaluation of metrics in alignment with current state processes | |||
| 7/15/2013 | 8 | 8 | 8 | Develop model in alignment with financial considerations. | |||
| 7/15/2013 | 8 | 8 | 8 | Review model with OQPS and refine | |||
| 8/1/2013 | 8 | 8 | 8 | Present proposed model to publics | |||
| 8/15/2013 | 8 | 8 | 8 | Refine model based upon comments from publics | |||
| 9/1/2013 | 8 | 8 | 8 | Final sign-off of model and submission to CMS | |||
| 6013 | Project Name: NYCOTB Division Lead: Health Reform and Health Insurance Exchange Integration Team Lead: Dawn M. Oliver Additional Staff: Kathleen Jackson, Rita Zink, Mark Malone Description: Implement a state only Medicaid benefit program for former NYC OTB retirees |
||||||
| 4/8/13 | P | P | P | Establish work team to create the benefit structure | |||
| 4/9/13 | P | P | P | Workgroup identifies system changes needed to WMS and eMedNY | |||
| 4/11/13 | P | P | P | Application and FAQ distributed to OTB retirees | |||
| 4/22/13 | P | P | P | eMedNY evolution project request and WMS system change request submitted | |||
| 5/6/13 | P | P | P | Client notice language drafted and submitted for legal review | |||
| 6/11/13 | P | P | P | 620 applications received from OTB retirees | |||
| 6/18/13 | P | P | P | WMS and eMedny system changes scheduled for implementation | |||
| 7/9/13 | 8 | 8 | 8 | Complete Eligibility determinations | |||
| 7/10/13 | 8 | 8 | 8 | OTB retiree Medicaid benefits active | |||
| 6014 | Project Name: Family Health Plus Program discontinuation Division Lead: Bureau of Medicaid Enrollment & Exchange Integration Team Lead: Kathleen Johnson Additional Staff: Judith Layton and Peggy Noonan Description: Family Health Plus Program is ending 12/31/2014, no new enrollment after 12/31/2013 |
||||||
| PART 1 | |||||||
| Policy and Procedure | |||||||
| 5/20/13 | P | P | P | Complete preliminary review of policy issues | |||
| 10/1/13 | 8 | 8 | 8 | Submit draft Administrative Directive (ADM) for clearance | |||
| 10/1/13 | 8 | 8 | 8 | Draft Medicaid Update Article for clearance | |||
| 10/15/13 | 8 | 8 | 8 | Submit changes to 1115 waiver amendment | |||
| 11/1/13 | 8 | 8 | 8 | Update MARG | |||
| 11/1/13 | 8 | 8 | 8 | Update trainings | |||
| 12/1/13 | 8 | 8 | 8 | Update AccessNY application | |||
| 12/15/13 | 8 | 8 | 8 | Issue ADM | |||
| 12/15/13 | 8 | 8 | 8 | Issue Medicaid Update Article | |||
| 12/31/13 | 8 | 8 | 8 | Eliminate FHPlus brochures | |||
| 1/1/14 | 8 | 8 | 8 | Cease acceptance of new applications | |||
| Take final steps to discontinue FHPlus- include in 1115 Waiver Amendment | |||||||
| 5/29/13 | P | P | P | Develop Tribal notification letter | |||
| 5/29/13 | P | P | P | Develop Public Notice | |||
| 5/30/13 | P | P | P | Submit Tribal notification letter for approval | |||
| 5/30/13 | P | P | P | Submit Public Notice for approval/clearance | |||
| 7/1/13 | 8 | 8 | 8 | Mail Tribal notification letter | |||
| 8/1/13 | 8 | 8 | 8 | Submit Public Notice for publication | |||
| 9/1/13 | 8 | 8 | 8 | Receive/Respond to Tribal and Public comments | |||
| 11/1/13 | 8 | 8 | 8 | Submit changes to 1115 waiver amendment | |||
| Internet | |||||||
| 1/1/15 | 8 | 8 | 8 | Disable website | |||
| Systems | |||||||
| Heart/WMS | |||||||
| 3/1/13 | P | P | P | Explore necessary system changes (cease acceptance of new applications) | |||
| 4/4/13 | P | P | P | Submit System Change Request Form | |||
| 4/4/13 | P | P | P | Finalize System Change requirements | |||
| 4/24/13 | P | P | P | Finalize System Action request | |||
| 11/30/13 | 8 | 8 | 8 | Development/Coding changes | |||
| 12/23/13 | 8 | 8 | 8 | Unit testing | |||
| 12/31/13 | 8 | 8 | 8 | User acceptance | |||
| CNS | |||||||
| 6/12/13 | P | P | P | Explore CNS notice issues | |||
| 11/21/13 | 8 | 8 | 8 | Eliminate/Revise CNS notices | |||
| PART 2 | |||||||
| Move S/CC into managed care & Transition Parents at Renewal | |||||||
| Policy and Procedure | |||||||
| 5/20/13 | P | P | P | Complete preliminary review of policy issues | |||
| 10/1/13 | 8 | 8 | 8 | Submit draft GIS for clearance- S/CC flip into Medicaid Managed Care | |||
| 12/15/13 | 8 | 8 | 8 | Issue GIS | |||
| 12/31/13 | 8 | 8 | 8 | Amend 1115 Waiver STC (if necessary) | |||
| 12/31/13 | 8 | 8 | 8 | Move parents/caretake relatives out of FHPlus into MAGI | |||
| Systems | |||||||
| WMS | |||||||
| 1/1/13 | P | P | P | Explore necessary system changes- move recipients into other coverage | |||
| 2/13/13 | P | P | P | Submit System Change Request From | |||
| 5/28/13 | P | P | P | Finalize System Change requirements | |||
| 6/3/13 | P | P | P | Finalize System Action request | |||
| 11/30/13 | P | P | P | Development/coding changes | |||
| 12/23/13 | 8 | 8 | 8 | Unit testing | |||
| 12/31/13 | 8 | 8 | 8 | User acceptance | |||
| CNS | |||||||
| 6/12/13 | P | P | P | Explore CNS notice issues | |||
| 11/21/13 | 8 | 8 | 8 | Finalize and submit CNS notices | |||
| PART 3 | |||||||
| Repeal of FHPlus Program | |||||||
| Policy and Procedure | |||||||
| 5/20/13 | P | P | P | Complete preliminary review of policy issues | |||
| 12/31/13 | 8 | 8 | 8 | Final Waiver Approval | |||
| Internet | |||||||
| 1/1/15 | 8 | 8 | 8 | Disable FHPlus mailbox | |||
| PART 4 | |||||||
| Premium "wrap" for parents/caretakers income 138-150% | |||||||
| 5/15/13 | P | P | P | Discussion with CMS | |||
| 5/16/13 | P | P | P | Discussion with CSS | |||
| 10/1/13 | 8 | 8 | 8 | Negotiate STC for Waiver | |||
| 12/31/13 | 8 | 8 | 8 | Final Waiver approval | |||
| MRT Project # |
Date | Schedule | Budget | Risk | Project/Task Description | State Savings 2012-13($millions) | Information for Team Leads |
| Key | P = Completed 8 = On Track ▲ = Caution T = Alert _ = Unknown | ||||||
| 6101 | Project Name: Health Homes Supportive Housing Pilot Project Division Lead: Lana Earle & Mark Kissinger Additional Staff: Barry Kinlan, Becky Corso, Gino Santabarba Description: Funding will support $5 million of rent and service subsidies to supportive housing providers to house and serve unstably housed high cost Medicaid recipients enrolled in Health Homes. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 6/17/13 | P | P | P | Participated in an internal meeting to discuss funding distributions (RFP, RFA, single source procurement) | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| 6102 | Project Name: OMH Supported Housing Services Supplement Division Lead: Bob Myers, Moira Tashjian (OMH) Description: Funding will support rent and service subsidies to supplement OMH Supported Housing in order to provide necessary day-to-day continuity of place-based, wraparound support services through a flexible critical time intervention approach. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| 6103 | Project Name: Homeless Senior Placement Pilot Project Division Lead: Linda Glassman (OTDA) Description: Funding will support rent and service subsidies to seniors currently residing within the shelter system. Funding will transition this population into the community. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 5/28/13 | P | P | P | Internal meeting to discuss program development | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| 6104 | Project Name: Health Home HIV + Rental Assistance Pilot Project Division Lead: Joseph Losowski (AIDS Institute) Description: Funding will support rental assistance for homeless and unstably housed health home participants diagnosed with HIV infection but medically ineligible for the existing HIV-specifc enhanced rental assistance program for New Yorkers with AIDS or advanced HIV-illness. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 6/17/13 | P | P | P | Participated in an internal meeting to discuss funding distributions (RFP, RFA, single source procurement) | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| 6105 | Project Name: Senior Supportive Housing Pilot Project Team Lead: Mark Kissinger, Liz Misa, Rebecca Corso, Gino Santabarbara Description: Funding will support capital and supportive services to enable low-income seniors to remain in the community. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 6/17/13 | P | P | P | Participated in an internal meeting to discuss funding distributions (RFP, RFA, single source procurement) | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| 6106 | Project Name: Step-Down/Crisis Residence Capital Conversion Pilot Project Division Lead: Bob Myers, Moira Tashjian (OMH) Description: Funding will support capital and operating funding to allow for a specified number of existing community residential service providers to convert a certain number of beds in crisisor step-down service units. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 6/14/2013 | P | P | P | Draft RFP for 12 to 15 agencies to provide existing providers to expand or convert a certain # of units for individuals in need of crisis stabilization/hospital diversion or hospital step-down. | |||
| 8/15/2013 | 8 | 8 | 8 | Release RFP | |||
| 10/15/13 | 8 | 8 | 8 | Announce awards | |||
| 12/1/13 | 8 | 8 | 8 | Begin contracts | |||
| 6107 | Project Name: Nursing Home to Independent Living Rapid Transition Division Lead: Mark Kissinger, Liz Misa, Rebecca Corso, Gino Santabarbara Description: Funding will support rent and service subsidies to offer individuals with mobility impairments or other severe physical disabilities an alternative pathway to community living. |
||||||
| 5/17/2013 | P | P | P | Participated in a call with Agency staff and circulated the work plan | |||
| 6/17/13 | P | P | P | Participated in an internal meeting to discuss funding distributions (RFP, RFA, Sole Source Contract) | |||
| 7/1/13 | 8 | 8 | 8 | Determine funding distribution mechanism | |||
| MRT Project # |
Date | Schedule | Budget | Risk | Project/Task Description | State Savings 13-14 ($millions) |
Information for Team Leads |
| Key | Completed, On Track, Caution, Alert | ||||||
| P = Completed 8 = On Track ▲ = Caution T = Alert | |||||||
| 6201 | Project Name: Activating Ordering/Prescribing/Referring/Attending Edits Division Lead: OHIP Operations Team Lead: Jonathan Bick Additional Staff: Nancy Tumey Description: Savings identified through implementation of ACA requirement that ordering/referring practitioners be enrolled in Medicaid for FFS claims to be paid. |
||||||
| 5/20/13 | P | P | P | Post FAQs on web | |||
| 7/1/2013 7/9/13 |
8 | 8 | 8 | Conduct Webinar to encourage and facilitate enrollment | |||
| 7/1/13 | 8 | 8 | 8 | Review current claims activity (excluding pharmacy) against new edits | |||
| 7/15/13 | 8 | 8 | 8 | Reach out to the subset of providers whose current claims activity reveals the greatest potential of future claims denials | |||
| 7/1/13 | 8 | 8 | 8 | Issue a Medicaid Update article. Outline pend and release process, encourage enrollment, highlight the FAQ document and restate that edits will be set to deny in October. | |||
| 8/1/13 | 8 | 8 | 8 | Reach out to OOS hospitals with whom Medicaid has entered into special pricing arrangements | |||
| 8/1/13 | 8 | 8 | 8 | Begin pend and release | |||
| 9/1/13 | 8 | 8 | 8 | Determine rollout schedule of edits/claim type to deny | |||
| 9/1/13 | 8 | 8 | 8 | Finalize rate code bypass for services ordered/referred by non-enrollable professionals | |||
| 9/1/13 | 8 | 8 | 8 | eMedNY listerv on pend and release, rollout of edits | |||
| 10/1/13 | 8 | 8 | 8 | Begin setting edits to deny | |||
| 6202 | Project Name: Incontinence Supply Contractor Division Lead: OHIP Operations Team Lead: Kevin Hepp Additional Staff: Jonathan Bick, Debby Henderson, William Hamilton Description: Achieve savings through bulk purchasing, rebates, and/or additional utilization management inititatives |
$.8 | |||||
| 4/1/13 | P | P | P | Obtain statutory authority | |||
| 6/15/13 7/15/13 | 8 | 8 | 8 | Publish RFI to solicit industry feedback on approaches | |||
| 7/22/2013 8/22/13 | 8 | 8 | 8 | Complete review of RFI responses and recommend approach | |||
| 8/1/2013 9/1/13 | 8 | 8 | 8 | Contracting/procurement approach determined | |||
| 9/1/13 10/1/13 | 8 | 8 | 8 | Determine feasibiliy of combining effort with exisiting or future state/local government procurements | |||
| 9/1/2013 10/1/13 | 8 | 8 | 8 | Initiate procurement activities | |||
| 10/1/2013 11/1/13 | 8 | 8 | 8 | Initiate review of proposals | |||
| 10/15/13 11/15/13 | 8 | 8 | 8 | Select contractor(s) | |||
| 10/22/13 11/22/13 | 8 | 8 | 8 | Initial provider notification | |||
| 11/15/2013 12/15/13 | 8 | 8 | 8 | Approval of contract(s) | |||
| 1/1/14 2/1/13 | 8 | 8 | 8 | Begin implementing initiative | |||
| 6203 | Project Name: Increase Manual Review of Claims Division Lead: OHIP Operations Team Lead: Ellen Harris Additional Staff: Jonathan Bick Description: Hiring package of 5 claims reviewers to increase cost effective manual review of FFS claims. |
$8.25 | |||||
| 3/18/13 | P | P | P | Waiver package submitted to DOB | |||
| 6/14/13 | 8 | 8 | 8 | DOB approval of waiver package | |||
| 6/28/13 | 8 | 8 | 8 | Positions posted | |||
| 7/15/13 | 8 | 8 | 8 | Begin interviews | |||
| 8/02/13 | 8 | 8 | 8 | Nominate candidates | |||
| 8/14/13 | 8 | 8 | 8 | Offer positions | |||
| 8/29/13 | 8 | 8 | 8 | Staff begin training period | |||
| 11/29/13 | 8 | 8 | 8 | Initial training period complete | |||
| 12/31/13 | 8 | 8 | 8 | First report on savings results | |||
| 6204 | Project Name: Hearing Aid Administrative Streamlining Division Lead: OHIP Operations Team Lead: Erin K. Finigan Additional Staff: Debby Henderson, Jonathan Bick, TBD Description: Propose regulation change to facilitate transition from paper to electronic billing to reduce administrative burden on providers and the State. Develop maximum fees based on an average cost of products representative of each type of hearing aid. This will allow automated processing of claims and is consistent with current regulations and procedures for complex wheelchairs and other equipment as well as other payors nationwide. |
$0.25 | |||||
| 05/17/13 | P | P | P | Amendment packet submitted to DLA | |||
| 08/31/13 | 8 | 8 | 8 | Obtain approval for amendment proposal | |||
| 10/31/13 | 8 | 8 | 8 | Obtain feedback from provider and beneficiary stakeholder groups | |||
| 11/30/13 | 8 | 8 | 8 | Establish MRAs for each code | |||
| 12/15/13 | 8 | 8 | 8 | Update eMedNY system to reflect fees | |||
| 12/15/13 | 8 | 8 | 8 | Update Hearing aid fee schedule | |||
| 12/15/13 | 8 | 8 | 8 | Educate staff | |||
| 12/31/13 | 8 | 8 | 8 | Educate provider community | |||
| 01/31/14 | 8 | 8 | 8 | Begin implementing initiative | |||
no reviews yet
Please Login to review.