180x Filetype PDF File size 0.42 MB Source: www.lumen.luc.edu
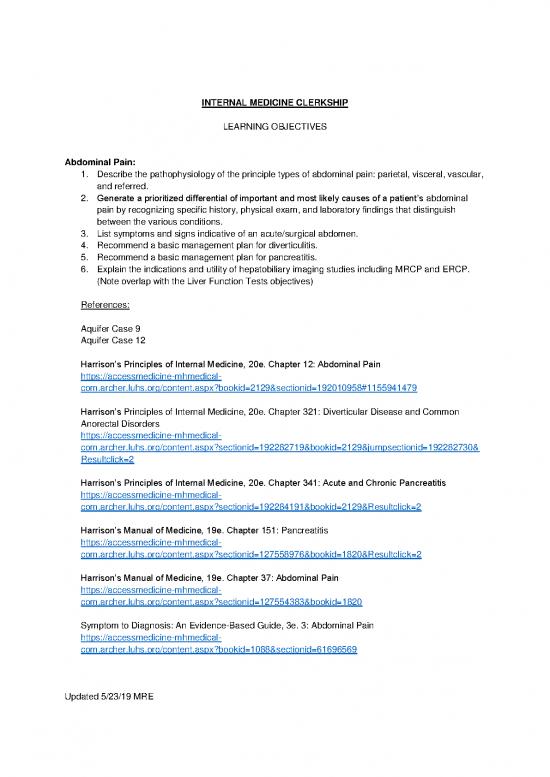
INTERNAL MEDICINE CLERKSHIP
LEARNING OBJECTIVES
Abdominal Pain:
1. Describe the pathophysiology of the principle types of abdominal pain: parietal, visceral, vascular,
and referred.
2. Generate a prioritized differential of important and most likely causes of a patient’s abdominal
pain by recognizing specific history, physical exam, and laboratory findings that distinguish
between the various conditions.
3. List symptoms and signs indicative of an acute/surgical abdomen.
4. Recommend a basic management plan for diverticulitis.
5. Recommend a basic management plan for pancreatitis.
6. Explain the indications and utility of hepatobiliary imaging studies including MRCP and ERCP.
(Note overlap with the Liver Function Tests objectives)
References:
Aquifer Case 9
Aquifer Case 12
Harrison’s Principles of Internal Medicine, 20e. Chapter 12: Abdominal Pain
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?bookid=2129§ionid=192010958#1155941479
Harrison’s Principles of Internal Medicine, 20e. Chapter 321: Diverticular Disease and Common
Anorectal Disorders
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=192282719&bookid=2129&jumpsectionid=192282730&
Resultclick=2
Harrison’s Principles of Internal Medicine, 20e. Chapter 341: Acute and Chronic Pancreatitis
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=192284191&bookid=2129&Resultclick=2
Harrison’s Manual of Medicine, 19e. Chapter 151: Pancreatitis
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=127558976&bookid=1820&Resultclick=2
Harrison’s Manual of Medicine, 19e. Chapter 37: Abdominal Pain
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=127554383&bookid=1820
Symptom to Diagnosis: An Evidence-Based Guide, 3e. 3: Abdominal Pain
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?bookid=1088§ionid=61696569
Updated 5/23/19 MRE
Acid-Base Disorders:
1. Identify and discuss the normal homeostatic mechanisms which maintain pH in the normal range.
2. Describe the principles of the Henderson-Hesselbach equation.
3. Describe the effect on pH of:
a. Metabolic acidosis.
b. Metabolic alkalosis.
c. Respiratory acidosis.
d. Respiratory alkalosis.
4. Discuss the renal and/or respiratory adaptation to the abnormalities in (3) above.
5. Calculate the anion gap and explain its relevance to determining the cause of a metabolic
acidosis.
6. Define and describe the pathophysiology of:
a. Simple and mixed acid-base disorders.
b. Respiratory acidosis and alkalosis.
c. Metabolic acidosis and alkalosis.
7. Discuss presenting signs and symptoms of the above disorders.
8. List the differential and identify the most common causes of respiratory acidosis, respiratory
alkalosis, non-anion gap metabolic acidosis, anion gap metabolic acidosis, and metabolic
alkalosis.
9. Discuss how altered mental status can contribute to electrolyte disorders.
10. Discuss tests to use in the evaluation of fluid, electrolyte, and acid-base disorders.
11. Predict acid-base abnormalities from the clinical picture.
12. Identify acid-base abnormalities that medicines can cause.
13. List and discuss indications for obtaining an arterial blood gas (ABG).
References:
Lecture: Acid-base disorders
Aquifer Case 26
Harrison’s Manual of Medicine, 19e. Chapter 1: Electrolytes/Acid-Base Balance
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=127553582&bookid=1820&Resultclick=2#1128781609
Harrison’s Principles of Internal Medicine, 20e. Chapter S1: Fluid and Electrolyte Imbalances and
Acid-Base Disturbances: Case Examples
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=192509786&bookid=2129&Resultclick=2
Symptom to Diagnosis: An Evidence-Based Guide, 3e. 4: Acid-Base Abnormalities
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?bookid=1088§ionid=61696804
Acute Renal Failure:
1. Compare and contrast the distinction between the three major pathophysiologic etiologies for
acute renal failure (ARF) based on history, urinalysis, urine studies, and radiological imaging:
a. Decreased renal perfusion (prerenal)
Updated 5/23/19 MRE
i. Hypovolemia.
ii. Decreased cardiac output.
iii. Systemic vasodilation.
iv. Renal vasoconstriction.
a. Intrinsic renal disease (renal)
i. Vascular lesions.
ii. Glomerular lesions.
iii. Interstitial nephritis.
iv. Intra-tubule deposition/obstruction.
v. Acute tubular necrosis (ATN).
b. Acute renal obstruction (postrenal)
i. Ureteral (e.g. tumors, calculi, clot, sloughed papillae, retroperitoneal fibrosis,
lymphadenopathy).
ii. Bladder neck (e.g. tumors, calculi, prostatic hypertrophy or carcinoma,
neurogenic).
iii. Urethral (e.g. stricture, tumors, obstructed indwelling catheters).
2. Describe the metabolic consequences of significant reductions in renal function.
3. Describe the indications for dialysis.
4. Calculate the fractional excretion of sodium and/or the fractional excretion of urea and apply it to
distinguish between pre-renal and intrinsic renal disease causes of acute renal failure.
5. Develop an appropriate initial management plan for acute renal failure including volume
management, dietary recommendations, drug dosage alterations, electrolyte monitoring, and
indications for dialysis.
6. Interpret a urinalysis, including microscopic examination for casts, red blood cells, white blood
cells, and crystals. (Note overlap with the Renal Tests objectives)
7. Calculate the anion gap and generate a differential diagnosis for metabolic acidosis. (Note
overlap with the Acid-Base Disorders objectives)
8. Identify risk factors for contrast-induced nephropathy and recommend steps to prevent this
complication.
References:
Case Discussion: Acute Renal Failure
Aquifer Case 33
Harrison’s Principles of Internal Medicine, 20e. Chapter 304: Acute Kidney Injury
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=186950567&bookid=2129&Resultclick=2#1157019087
Harrison’s Manual of Medicine, 19e. Chapter 138: Acute Renal Failure
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?sectionid=127558544&bookid=1820&Resultclick=2
Symptom to Diagnosis: An Evidence-Based Guide, 3e. 28: Kidney Injury, Acute
https://accessmedicine-mhmedical-
com.archer.luhs.org/content.aspx?bookid=1088§ionid=61700156
Updated 5/23/19 MRE
Anemia/Complete Blood Count:
1. Be able to define and describe the classification of anemia based on red cell size:
a. Microcytic
i. Iron deficiency.
ii. Thalassemic disorders.
iii. Sideroblastic anemia.
iv. Lead toxicity/poisoning.
v. Anemia of chronic disease.
b. Normocytic
i. Acute blood loss.
ii. Hemolysis.
iii. Anemia of chronic disease (e.g. infection, inflammation, malignancy).
iv. Chronic renal insufficiency/erythropoietin deficiency.
v. Bone marrow suppression (e.g. bone marrow invasion, aplastic anemia).
vi. Hypothyroidism.
vii. Testosterone deficiency.
viii. Early presentation of microcytic or macrocytic anemia (e.g. early iron deficiency
anemia).
ix. Combined presentation of microcytic and macrocytic anemias.
c. Macrocytic
i. Ethanol abuse.
ii. B12 deficiency.
iii. Folate deficiency.
iv. Drug-induced.
v. Reticulocytosis.
vi. Liver disease.
vii. Myelodysplastic syndromes.
viii. Hypothyroidism.
2. Discuss the potential usefulness of the white blood cell count and platelet count when attempting
to determine the cause of anemia.
3. Discuss the meaning and utility of various components of the hemogram (e.g., hemoglobin,
hematocrit, mean corpuscular volume, and red cell distribution width).
4. Classify anemia into hypoproliferative and hyperproliferative categories using the reticulocyte
count/index.
5. Use information regarding the diagnostic utility of the various tests for iron deficiency (e.g., serum
iron, total iron binding capacity, transferring saturation, ferritin) when selecting a lab evaluation for
iron deficiency.
6. Identify key historical and physical exam findings in the patient with anemia.
7. Recognize common morphologic changes on a peripheral blood smear.
8. Develop a further evaluation and management plan for a patient with anemia.
9. Incorporate the complete blood count with the history and physical exam to prioritize a differential
diagnosis and management plan for a patient with anemia.
References:
Lecture: CBC / Anemia
Aquifer Case 19
Updated 5/23/19 MRE
no reviews yet
Please Login to review.